Sensory Processing Disorder Treatment: A Practical Guide
When we talk about effective sensory processing disorder treatment, we're really talking about a collection of therapies and smart strategies designed to help a child's brain make better sense of the world around them. The aim isn't to "cure" the disorder, but to give children the tools and support they need to feel calm, confident, and in control.
What Is Sensory Processing Disorder, Really?

Think of your child's brain as a busy traffic intersection. Sights, sounds, touch, and other sensory signals are the cars trying to get through. In a typical brain, a well-functioning traffic light keeps everything flowing smoothly. But for a child with Sensory Processing Disorder (SPD), that traffic light is on the fritz.
Sometimes, all the signals rush in at once, causing a massive pile-up. This is over-responsiveness. Other times, the signals don't seem to move at all, creating a frustrating gridlock. That's under-responsiveness.
This neurological "traffic jam" is the reason behind behaviours that can seem puzzling from the outside. A clothing tag might feel like sandpaper. A friendly pat on the back could feel like a shove. Or, they might not even register a scraped knee. It’s not a choice or misbehaviour; their brain is genuinely struggling to receive, sort, and react to information from the senses.
Telltale Signs of Sensory Dysregulation
Figuring out if your child is struggling with sensory processing is the first big step. The signs usually fit into two main camps, though it's common for kids to have a foot in both.
Over-Responsive (Hypersensitive) Signs:
- Extreme Reactions: Think big emotional meltdowns over loud sounds, bright lights, or strong smells.
- Aversion to Textures: They might refuse to wear certain clothes, avoid messy play like finger painting, or hate having their hands dirty.
- Picky Eating: Often, this isn't about the taste but the texture. They might have powerful reactions to mushy, crunchy, or slimy foods.
Under-Responsive (Hyposensitive) Signs:
- Constant Motion: This is the child who is always seeking more input—jumping, spinning, crashing into furniture, and climbing on everything.
- High Pain Threshold: They may not seem to notice bumps, bruises, or extreme temperatures that would bother other kids.
- Hands-On Explorer: A constant need to touch people and objects, sometimes without a great sense of personal space.
It's a game-changer when you start seeing these behaviours as a form of communication. Instead of asking, "How do I stop this?" you can ask, "What is my child's nervous system trying to tell me?" This shift from frustration to curiosity is where real solutions begin.
The True Goal of Treatment
The core purpose of sensory processing disorder treatment isn't to stamp out these sensory traits. It's to help the brain's "traffic light" work more efficiently. This process is often called sensory integration.
Effective therapy helps a child build up their tolerance for sensations they find overwhelming while also learning how to get the sensory input they crave in a safe and appropriate way. The result? Better focus, calmer emotions, and a greater ability to join in with school, play, and family life.
Here in Australia, we see a strong connection between sensory challenges and other developmental conditions. For instance, the number of children with autism spectrum disorder (ASD) who also have sensory processing difficulties is incredibly high—studies suggest it's somewhere between 45% and 96%. This overlap has rightly put a bigger focus on getting kids effective support as early as possible.
Once you understand the 'why' behind the challenges, you can find the right tools to help your child thrive. To learn more about how these needs show up day-to-day, you can explore our in-depth guide on how sensory needs can be covered.
Professional Therapies That Build Stronger Foundations

When you're looking for effective sensory processing disorder treatment, professional therapies are where you’ll find the most powerful support. These evidence-based approaches do more than just manage day-to-day challenges. Their real aim is to help rewire the brain, building stronger and more efficient neural pathways so a child can better organise and respond to the world around them.
For most families in Australia, this journey starts with a visit to an occupational therapist, or OT. OTs are experts in helping people of all ages participate in the essential activities—or "occupations"—of daily life. For a child, that means everything from playing with friends and learning at school to managing self-care like getting dressed or eating a meal.
The work an OT does for SPD is deeply personal and never one-size-fits-all. They’ll create a plan based on your child’s unique sensory profile, with the ultimate goal of helping them feel more regulated, capable, and confident in every part of their life.
The Power of Occupational Therapy and Sensory Integration
At the heart of most OT for SPD is a remarkable approach called Ayres Sensory Integration® (ASI). The best way to think of ASI is as a carefully guided workout for the nervous system, cleverly disguised as fun and games. An OT creates a purpose-built, safe environment—often called a "sensory gym"—filled with specialised equipment that gives a child the exact sensory input their brain is craving.
This isn’t about forcing a child to tolerate sensations they find awful. Far from it. It's about providing what therapists call the "just-right" challenge, nudging their brain to adapt and form new connections in a way that feels empowering, not overwhelming.
A core principle of ASI is that the child is in the driver's seat. Therapy is child-directed, which means the therapist follows the child's own motivation. When a child is intrinsically drawn to an activity, their engagement is authentic, making the hard work of building new neural pathways feel like pure, exciting play.
In a typical OT session using ASI, you might see a child:
- Swinging: A sensory swing provides powerful vestibular input, the sense that governs balance, movement, and spatial awareness.
- Crashing: Leaping into a giant crash pad or squeezing into a body sock delivers deep pressure, a type of input that has a profound calming and organising effect on the nervous system.
- Exploring Textures: Digging into a sensory bin filled with different materials, such as those from Little Potion Co, helps gently desensitise a child to textures they might otherwise find overwhelming.
Here in Australia, ASI is a highly respected and widely used approach. A review of local OT practices revealed that over 70% of therapists use sensory integration as a core part of their intervention for children with SPD. This widespread trust reflects a strong professional consensus on its power to create lasting, positive change. For a deeper look into the evidence, you can explore the findings on sensory-based interventions from an NDIS review.
A Team-Based Approach to Treatment
While OT is often the lead therapy, the best results usually come from a collaborative team. Other professionals bring their own expertise to the table, helping to address the many different ways SPD can impact a child’s life.
- Speech and Language Therapy: If a child’s sensory sensitivities are causing feeding difficulties—like avoiding certain food textures—a speech pathologist can be a game-changer. They use structured, playful techniques to gradually and safely introduce new foods, making mealtimes less of a battle.
- Behavioural Therapies: A psychologist or behaviour therapist can arm a child with practical coping strategies. They might teach them how to recognise the early warning signs of sensory overload and use calming techniques, like deep breathing or finding a quiet space, before things get overwhelming.
To see how these therapies fit together, take a look at the table below.
Comparing Key Therapeutic Approaches for SPD
This table provides a snapshot of how different professionals contribute to a holistic treatment plan for SPD, highlighting their unique goals and methods.
| Therapy Type | Primary Goal | Common Activities & Tools |
|---|---|---|
| Occupational Therapy | Improve the brain's ability to process sensory input and enhance participation in daily activities. | Using a sensory swing, weighted blankets, obstacle courses, tactile play, and creating sensory diets. |
| Speech Therapy | Address feeding aversions and communication challenges related to sensory sensitivities. | Food chaining, texture exploration games, and developing social communication skills in group settings. |
| Behavioural Therapy | Teach practical coping skills and emotional regulation strategies for overwhelming situations. | Role-playing social scenarios, creating visual schedules, and practising mindfulness techniques. |
When these professionals work together, they create a comprehensive support network that addresses your child's needs from every angle. This kind of integrated sensory processing disorder treatment doesn't just help children cope; it gives them the foundational skills they need to truly thrive.
Turning Your Home into a Sensory Haven

While professional therapy is the bedrock of any solid sensory processing disorder treatment plan, the real magic happens when you bring those strategies home. The goal isn't to turn your house into a clinic, but to weave sensory smarts into the fabric of your everyday life.
It's all about making small, thoughtful adjustments that help your child’s nervous system find its 'just right' state. This shifts your home from being a place of potential sensory landmines into a genuine sanctuary, making daily routines smoother and less stressful for the whole family.
What Is a Sensory Diet?
One of the most valuable concepts your occupational therapist (OT) will share is the "sensory diet." Don't worry, it has nothing to do with food!
A sensory diet is a carefully planned schedule of activities, personalised to your child, that provides the specific sensory input their brain needs to stay calm, alert, and organised throughout the day. Think of it like a nutritional diet for the nervous system.
A sensory diet is all about being proactive, not reactive. It’s the difference between helping your child do five minutes of jumping before school to get focused, versus trying to manage a full-blown meltdown after a long, overwhelming day.
Your OT will work with you to build a custom plan, but here’s what a sensory diet might look like in action:
- Morning Wake-Up: Start the day with deep pressure, like big bear hugs or being rolled up tightly in a blanket like a burrito.
- Before School: Get them involved in "heavy work" to ground their body. This could be carrying their own school bag or pushing a laundry basket to their room.
- After School: Burn off pent-up energy in a structured way with a sensory swing or some time on the trampoline.
- Evening Wind-Down: Prepare the brain for sleep with calming music, the gentle motion of a jellyfish lamp, or a warm bath.
Creating a Calm-Down Corner
Every child benefits from having a safe place to retreat to when the world feels too loud, too bright, or just plain too much. A designated calming corner gives your child a predictable, safe spot to go when they feel overwhelmed and need to regulate their emotions. Thoughtfully designed sensory spaces are key.
This doesn't have to be an entire room. It can be a cosy nook in their bedroom or a quiet spot in the living area. The key is to stock it with items that offer soothing sensory input. A brilliant and easy way to create an instant retreat is with a pop-up tent, like this block-out sensory tent, which immediately reduces distracting sights and sounds.
Inside this space, you could add:
- A pair of noise-cancelling earmuffs for kids to mute household noise.
- A small basket of tactile fidgets or a soft Warmie to keep hands busy.
- A weighted blanket or a comforting weighted animal toy for that grounding deep pressure.
Small Environmental Tweaks, Big Impact
Beyond a dedicated calm-down corner, you can make simple changes throughout your home that dramatically reduce the overall sensory 'noise'. These modifications lower the constant demand on your child's nervous system, making it easier for them to cope.
Consider swapping harsh overhead lights for night lights with warm bulbs or installing dimmer switches to control the brightness. Another game-changer is reducing visual clutter. Simply organising toys into labelled bins and keeping surfaces as clear as possible can create a profoundly calmer atmosphere.
By thoughtfully shaping your environment, you're not just decorating—you're embedding therapeutic support right into your home, reinforcing the skills learned in therapy and empowering your child to feel safe and successful.
Using Sensory Tools to Support Regulation
While professional therapies lay the essential groundwork for managing sensory challenges, the right tools at home and school are what truly bring those new skills to life. Sensory tools might look like toys, but they're so much more. Think of them as purposeful aids, carefully designed to give a child’s nervous system the specific input it needs to calm down, focus, and feel more organised.
Understanding the ‘why’ behind each tool is what makes all the difference. It’s not about just filling a box with cool gadgets; it's about knowing exactly which item provides the right kind of sensory feedback at the right moment.
For a child who is constantly on the move, a structured activity can be incredibly grounding. For another who gets overwhelmed by noise and crowds, a calming tool can be a genuine lifeline. These items aren't just add-ons; they are a vital part of a successful sensory processing disorder treatment plan.
Tactile and Deep Pressure Tools
When most people think of sensory aids, tactile and deep pressure tools are often what come to mind first. They provide input that can be profoundly calming and organising for a nervous system that’s feeling a bit scattered or revved up.
Deep pressure, in particular, is a game-changer. It works by tapping into the body's parasympathetic nervous system—the part responsible for that "rest and digest" feeling. Imagine the comforting security of a really good, firm hug. That’s deep pressure in action. This sensation can help lower a child’s heart rate and slow their breathing, bringing on a real sense of security and calm.
Here’s how different tools deliver that feeling:
-
Weighted Items: Things like weighted blankets or cuddly weighted animal toys provide a sustained, gentle pressure that drapes over the body. The Neptune Blanket, for example, is specifically designed to offer this steady, calming input, making it perfect for settling down at bedtime or during quiet time.
-
Fidgets: It’s a common myth that fidgets are just a distraction. In reality, they offer a quiet, focused outlet for busy hands. This simple act frees up the brain to concentrate on other things, like listening to the teacher or finishing a task. Brands like Kaiko fidgets and squishy Needohs come in a huge range of textures and resistances to meet different tactile preferences.
Visual and Auditory Tools
For many kids with SPD, the world can be a visually and audibly overwhelming place. The good news is that we can use these same senses to create calm and focus when we introduce the right kind of input. The goal is to swap out chaotic, unpredictable sensations for something rhythmic, predictable, and soothing.
Think about a busy classroom with flickering fluorescent lights and constant movement—it’s a recipe for overload. But a gentle, predictable visual like a lava lamp can help the brain filter out all that background noise and find a single point of focus.
Sensory tools are not a reward or a punishment. They are a legitimate support, just like glasses for someone who can't see clearly. Providing the right tool is about giving a child what their nervous system needs to function at its best.
Here are a few examples of helpful visual and auditory aids:
-
Soothing Lights: A mesmerising Jellyfish lamp or Jellyfish aquarium lamp offers slow, rhythmic movement that captures attention without being jarring. The gentle, predictable motion is incredibly calming, making it an excellent addition to a quiet corner or bedroom. In the same way, bubble tubes provide a relaxing visual with a gentle, humming sound.
-
Sound Reduction: For children who are sensitive to noise, noise cancelling earmuffs for kids are an absolute must-have. They turn down the volume in overwhelming places like shopping centres or school assemblies, helping to prevent sensory overload before it even starts.
Tools for Movement and Body Awareness
Some children seem to have a motor that just won’t quit. They are often seeking input for their vestibular system (which governs balance and movement) and their proprioceptive system (which tells them where their body is in space). Giving them safe and appropriate ways to get this input is a cornerstone of any good sensory diet.
Instead of trying to make them stop moving, our goal is to help them channel that energy productively. This kind of input can be highly regulating and, paradoxically, can actually improve their ability to sit still and focus later on.
-
Active Play: A sensory swing is brilliant because it offers both gentle, linear swinging and more alerting rotational movement, so it can be adapted to be either calming or energising depending on what a child needs.
-
Building and Logic: This is where creative construction toys really shine. Building with Magnatiles or designing a run with Gravitrax requires focus, problem-solving, and fine motor skills. It’s a fantastic way to channel mental and physical energy into a structured, rewarding task. Even familiar characters from Bluey merchandise or educational favourites like Numberblocks can be used to draw a child into purposeful, focused play.
Sensory products aren't just toys; they are carefully selected aids that serve a specific purpose in a child's sensory diet. Choosing the right one means understanding what sensory system it supports.
Guide to Sensory Products and Their Purpose
| Product Category | Examples | Primary Sensory Benefit |
|---|---|---|
| Deep Pressure | Weighted blankets, weighted lap pads, compression clothing | Calming the nervous system, improving body awareness (proprioceptive) |
| Tactile Fidgets | Kaiko fidgets, Needohs, textured balls | Providing a discreet outlet for restless hands, improving focus (tactile) |
| Movement | Sensory swings, wobble boards, therapy balls | Fulfilling the need for movement, improving balance (vestibular) |
| Visual | Jellyfish lamps, bubble tubes, liquid timers | Offering predictable, soothing visual input to help with focus and calm |
| Auditory | Noise-cancelling earmuffs, white noise machines | Reducing overwhelming sounds, creating a controlled auditory environment |
| Oral Motor | Chew necklaces, textured chew tools | Providing a safe outlet for chewing/biting needs, self-regulation (oral) |
| Construction | Magnatiles, Gravitrax, Airtoobz | Channelling energy into focused, goal-oriented play (proprioceptive/visual) |
Ultimately, the best sensory tools are the ones that meet your child's unique needs and are used consistently as part of a wider support strategy developed with your occupational therapist.
Navigating NDIS and Support Services in Australia
Figuring out the Australian support system to find the right sensory processing disorder treatment can feel overwhelming, but you're definitely not on this journey alone. With a clear roadmap, you can find your way to the resources your child needs to thrive.
The first port of call is usually your trusted GP. They can be a fantastic starting point, offering initial guidance and providing those crucial referrals to specialists like a paediatrician or an occupational therapist (OT) who can carry out a proper assessment.
Understanding the National Disability Insurance Scheme
The National Disability Insurance Scheme (NDIS) is Australia's primary system for supporting people with a permanent and significant disability. For many kids with severe sensory challenges, the NDIS is a lifeline, funding essential therapies and supports.
To qualify, a child needs to have a disability that's likely to be lifelong and significantly impacts their ability to do everyday things. While Sensory Processing Disorder isn't listed as a standalone condition for automatic NDIS access, it's often a critical part of a successful application, especially when it goes hand-in-hand with other diagnoses like autism.
The NDIS is all about funding what's "reasonable and necessary" to help someone reach their goals. This can cover everything from occupational therapy and assistive technology (like sensory tools) to training for parents so they can implement strategies at home.
The simple graphic below shows the powerful cycle of using sensory tools to help a child regulate their emotions—a core goal that many NDIS plans are built to support.
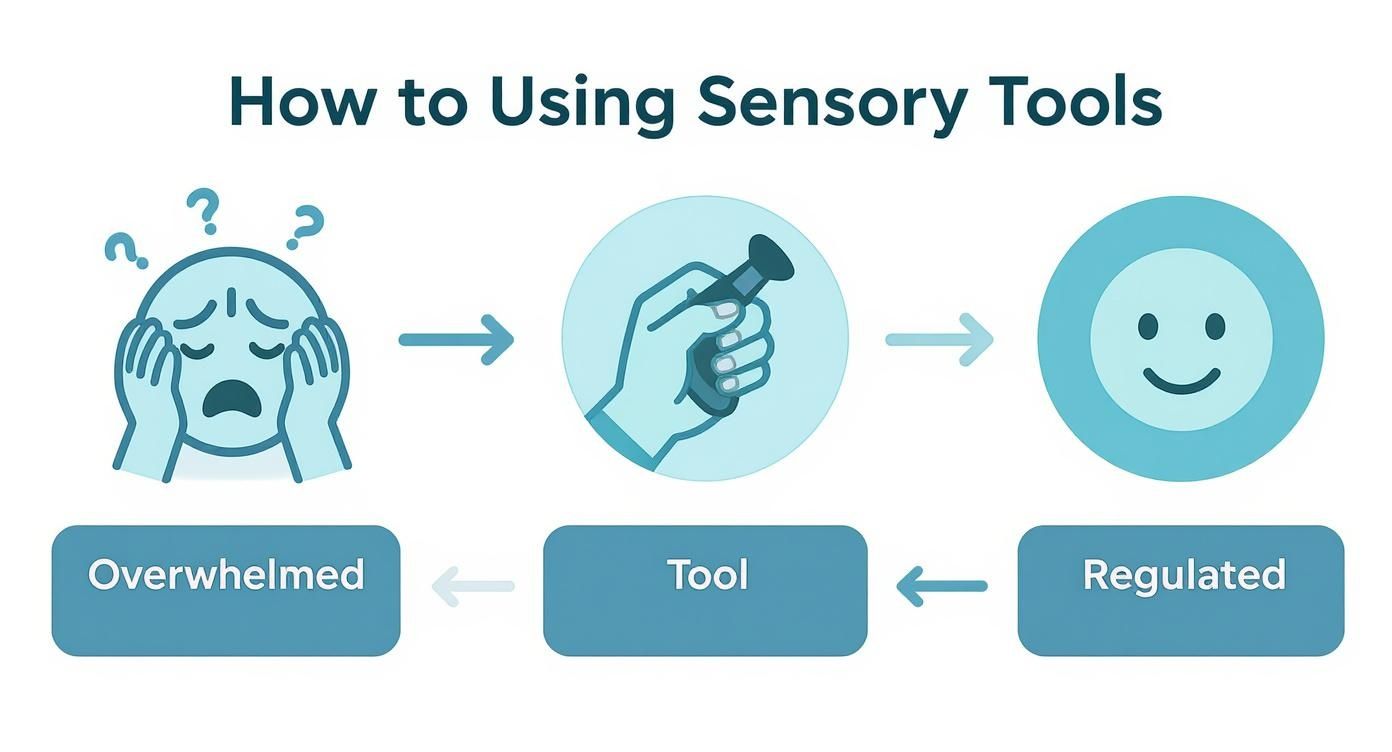
As you can see, the right tool at the right time can break the cycle of sensory overload and gently guide a child back to a state of calm. It's a perfect illustration of why these supports are so therapeutically valuable.
What Can the NDIS Fund?
If your child gets an NDIS plan, it will have funding split into different support categories. For a child with sensory needs, this funding can often be put towards:
- Therapeutic Supports: This is for ongoing sessions with professionals like an occupational therapist, speech pathologist, or psychologist.
- Consumables: This category can cover the cost of smaller, everyday sensory items like fidgets or therapeutic putty.
- Assistive Technology: Bigger or more specialised equipment, like a sensory swing or weighted blankets, usually falls under this budget.
Your NDIS planner or Local Area Coordinator (LAC) is there to help you figure out how to best use the funding in your plan to get the supports that will make a real difference for your child.
Accessing Other Supports in Australia
Beyond the NDIS, there are other pathways to get help. It’s always worth checking your private health insurance policy, as many plans offer rebates for allied health services like occupational therapy.
Schools are also getting much better at supporting students with sensory needs. Many have their own support staff and are able to create a more inclusive sensory classroom environment. Working closely with your child's school is key to making sure everyone is on the same page, creating consistency between home and the classroom.
Here in Australia, these kinds of interventions are widely recognised and respected. Sensory-based supports have become a standard, evidence-backed approach, and there are established frameworks to guide best practices in both schools and clinics. You can read more about the background of sensory interventions in Australia to get a better sense of their long-standing role in supporting children.
Your Questions Answered: Navigating SPD Treatment
Stepping into the world of sensory processing disorder treatment can feel overwhelming, and it’s completely natural to have a lot of questions. As a parent, you’re your child’s biggest advocate, and getting clear, straightforward answers is the first step to feeling confident on this journey. Let's tackle some of the most common questions we hear from families just like yours.
How Is Sensory Processing Disorder Different from ADHD?
This is probably one of the most frequent questions we get, and it’s a brilliant one. There’s a lot of overlap in what you might see on the surface—trouble concentrating, high energy levels, and big emotional reactions—but the 'why' behind the behaviour is often worlds apart.
Think of two kids who can’t seem to sit still in their chairs. The child with ADHD might be driven by an internal engine that’s always revving, a product of how their brain manages impulse control and attention. But the child with SPD might be squirming because the tag on their shirt feels like sandpaper, the humming from the fluorescent lights is painfully loud, or their body is craving deep pressure just to feel where it is in space.
A simple way to think about it: ADHD can be like the brain's "air traffic controller" having a hard time directing the planes, while SPD is more like the "communications tower" getting garbled signals from the start.
This is why a thorough assessment by a professional who truly understands both is so critical. It ensures your child gets support that targets the root cause, not just the symptom.
How Long Will Therapy for SPD Take?
There’s no magic number here. The timeline for therapy is as unique as your child is. It really depends on their specific sensory profile, how significant their challenges are, and how consistently the strategies are practiced both inside and outside the therapy room.
The goal isn't to "cure" SPD—it’s a lifelong neurological difference. Instead, therapy is all about empowerment. We're working to help your child’s brain build stronger, more efficient pathways for processing sensory information. More importantly, we're giving them a toolbox of strategies they can use for the rest of their lives to manage their needs.
Progress is often a series of small but mighty wins. It's the moment they try a new food without a meltdown, or successfully navigate a noisy birthday party using their noise cancelling earmuffs for kids. That’s when you know you’re on the right track.
Can My Child Just "Outgrow" Their Sensory Challenges?
While it’s true that kids develop new coping skills as they mature, SPD isn't something they simply leave behind like a pair of shoes they've outgrown. It's a fundamental part of their wiring. Waiting it out often means missing a crucial window where we can make the biggest impact.
Early and consistent sensory processing disorder treatment is so powerful because a young brain is incredibly flexible—what we call neuroplasticity. Therapy helps lay down the foundational skills a child needs to navigate a world that isn't always built for their nervous system. These skills become the bedrock that supports them as they face more complex classrooms, friendships, and social situations down the road.
Are Sensory Toys Just a Distraction, or Do They Genuinely Help?
This is a common misconception! When used with intention, sensory tools are far more than just distracting toys; they are powerful, purpose-built aids for self-regulation. Think of them as the practical, hands-on part of your child’s therapy plan.
An Occupational Therapist will help you build what's called a "sensory diet," and these tools are the 'ingredients'. Each one is chosen to provide a specific type of input that a child's nervous system needs to feel calm, focused, and organised.
- To Help with Focus: A discreet tactile tool like a Kaiko fidget or a squishy Needoh can give busy hands a job, which paradoxically frees up the brain to listen and learn in class.
- To Bring a Sense of Calm: The deep, grounding pressure from a Neptune Blanket or one of the many weighted animals toys can feel like a firm, reassuring hug, sending a powerful "it's okay" signal to the nervous system.
- To Help During a Meltdown: When a child is completely overwhelmed, the slow, predictable motion of a Jellyfish lamp or bubble tubes can provide a soothing visual anchor to help them come back down.
- To Encourage Play and Skill-Building: Building with Magnatiles or designing a marble run with Gravitrax isn't just play. It channels a child's energy into a task with a goal, building motor skills, focus, and confidence all at once.
From a cuddly Warmie to a collection of engaging fidgets, these tools are essential for creating supportive sensory spaces at home and in a sensory classroom. When you understand their purpose, you can help your child use them not as a distraction, but as a genuine support to help them thrive.
At The Sensory Poodle, we know that having the right tools makes all the difference. We've carefully selected a range of high-quality, therapist-approved sensory toys in Australia, from calming weighted blankets to engaging fidgets. Discover our full range of sensory solutions today and find the perfect supports to help your child on their journey.


